Living With Fibromyalgia: What It Feels Like, What Helps, and How to Care for Your Body Gently
I Didn’t Know My Body Was in Survival Mode — Until It Never Came Back Down
For a long time, I thought I was just tired.
Tired in a way sleep didn’t fix. Sore in a way stretching didn’t touch. Foggy in a way that made me question myself more than my health. I kept showing up — working, functioning, pushing — while quietly negotiating with a body that felt heavier every year. Some days the pain was dull and manageable. Other days it felt loud, demanding, and impossible to ignore. And yet, from the outside, I looked fine.
It took time — and a lot of unanswered questions — to learn that what I was experiencing had a name: fibromyalgia.
Not a phase. Not stress alone. Not something I could power through.
A real, chronic condition that affects how the nervous system processes pain, fatigue, sleep, and cognition.
If you’re here because your body feels unfamiliar…
If you’ve been told “everything looks normal” while nothing feels normal…If you’re tired of explaining pain you can’t point to —
This article is for you.
I’m going to walk you through what fibromyalgia actually is, how it’s diagnosed, what helps manage it, and what living with it really looks like — blending medical understanding with lived experience, because one without the other is incomplete.
Everything You Need to Know About Fibromyalgia
A real explanation, without the fluff — and what living with it actually feels like
Fibromyalgia isn’t something you casually “learn about.”
It’s something you experience — often quietly, often misunderstood, and often while still showing up for life.
If you’re here because you live with fibromyalgia, or because someone close to you does, I want to be clear from the start: this condition is real, complex, and far more than “aches and pains.”
This article breaks down what fibromyalgia actually is, how it’s diagnosed, what helps manage it, and what daily life can look like — blending medical facts with lived experience, because both matter.
What Fibromyalgia Really Is
Fibromyalgia is a chronic neurological pain condition that affects how the brain and nervous system process pain signals. In simple terms, the body experiences pain more intensely and more persistently than it should.
According to the Centers for Disease Control and Prevention (CDC), fibromyalgia commonly includes widespread pain, fatigue, sleep problems, mood disturbances, and difficulty with memory or concentration (often called “fibro fog”).
This isn’t imagined pain. It isn’t weakness. And it isn’t something you can think your way out of.
It’s a nervous system that’s stuck in overdrive.
Common Fibromyalgia Symptoms (That Don’t Always Show on the Outside)
Fibromyalgia doesn’t look the same for everyone, but many people experience some combination of:
• Widespread muscle and joint pain
• Deep, persistent fatigue that rest doesn’t fix
• Stiffness, especially in the morning
• Poor or non-restorative sleep
• Brain fog — trouble focusing, remembering, or processing
• Headaches or migraines
• Heightened sensitivity to light, sound, or touch
• Anxiety or depression
The hardest part? You can look completely “fine” while feeling anything but.
What Causes Fibromyalgia?
There is no single cause — and that’s part of why fibromyalgia is so misunderstood.
Medical research suggests fibromyalgia is linked to central sensitization, meaning the brain and spinal cord amplify pain signals instead of regulating them properly. Stress, trauma, illness, injury, or long-term nervous system overload can all play a role.
Poor sleep, chronic stress, and co-existing conditions (like IBS, migraines, or chronic fatigue symptoms) can make everything worse.
This condition isn’t about damage — it’s about dysregulation.
Why Fibromyalgia Is So Hard to Diagnose
There is no lab test that definitively diagnoses fibromyalgia. That alone causes years of frustration for many people.
Diagnosis is based on:
• Widespread pain lasting longer than 3 months
• Symptom patterns
• Medical history
• Ruling out other conditions with similar symptoms
The American College of Rheumatology (ACR) updated its diagnostic criteria to focus on symptom severity and pain distribution rather than pressure-point testing.
Translation?
Fibromyalgia is diagnosed by listening — not by a single blood test.
Treatment: What Actually Helps
There is no cure, but fibromyalgia can be managed. Most people do best with a layered approach rather than one solution.
Movement (Yes — But Gently)
Research consistently shows that low-impact aerobic movement and mixed exercise programs can improve pain and quality of life when introduced gradually.
This is not about pushing through pain.
It’s about supporting circulation, mobility, and nervous system regulation.
Think walking, stretching, water movement, light strength work — not punishment workouts.
Sleep Is Not Optional
Poor sleep worsens pain sensitivity. Improving sleep routines — even small changes — can significantly impact symptom severity.
Fibromyalgia and sleep issues often feed into each other, which means sleep support is part of treatment, not a luxury.
Stress & Nervous System Support
Stress doesn’t “cause” fibromyalgia — but it absolutely turns the volume up.
Mind-body tools like mindfulness, therapy, breathing practices, and pacing help calm the nervous system, which helps reduce symptom intensity over time.
Medication (When Appropriate)
Some people benefit from medications that support pain processing, sleep, or mood regulation. This is highly individual and should always be discussed with a provider who understands fibromyalgia.
Fibromyalgia Flares: When Everything Gets Louder
Flares happen. They’re often triggered by:
• Overexertion
• Poor sleep
• Stress
• Illness
• Weather changes
• Hormonal shifts
When a flare hits, the goal shifts from productivity to containment and care.
For many of us, that looks like:
• Scaling back without guilt
• Using heat, hydration, and easy nourishment
• Gentle movement instead of rest-only or push-through
• Earlier nights
• Less stimulation
Planning for flares doesn’t mean giving up — it means being realistic.
When to Seek Medical Attention
Always contact a healthcare provider if you experience:
• New neurological symptoms
• Chest pain or shortness of breath
• Unexplained weight loss or fever
• Sudden severe headaches
Fibromyalgia can overlap with other conditions, and new symptoms deserve attention.
Shop the Blog: Comfort & Support Favorites
These are quality-of-life supports, not treatments — things that make living with fibromyalgia more manageable.
• Heating pads or heated wraps
• Supportive pillows
• Sleep essentials (eye masks, blackout curtains)
• Gentle movement tools
• Pain & symptom journals
• Ergonomic desk supports
• Hydration tools
• Comfortable lounge wear
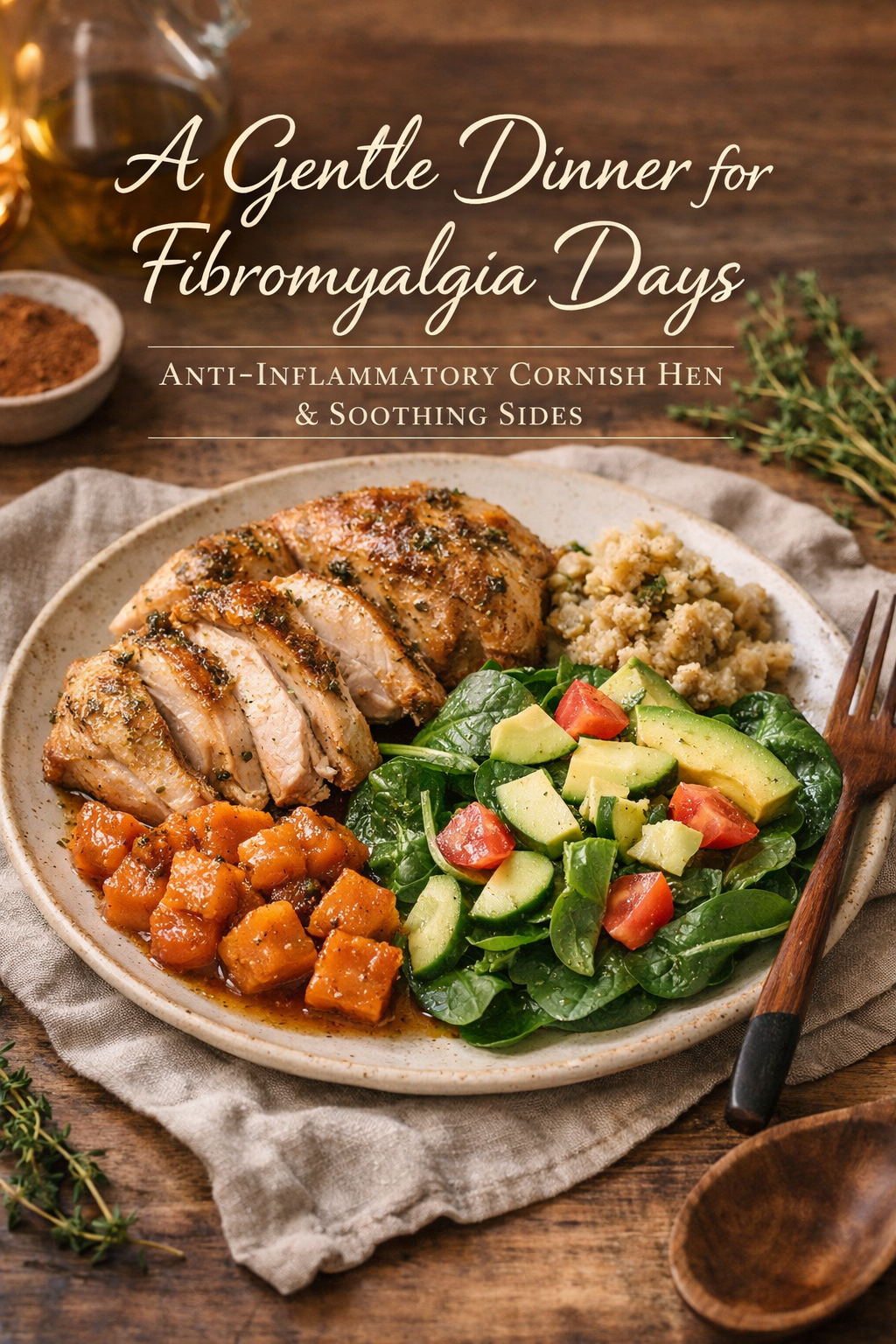
Care Doesn’t End With Information — It Continues With Nourishment
Living with fibromyalgia means learning that care happens in the small, quiet choices — especially when your body is already carrying enough.
One of the ways I support myself on low-energy days is through gentle, grounding meals that don’t overwhelm the nervous system or digestion.
If your body needs something warm, simple, and supportive tonight, I created something for you.
A Gentle Dinner for Fibromyalgia: Comfort, Nourishment, and Ease.
Make it stand out
Care Doesn’t End With Information — It Continues With Nourishment
Living with fibromyalgia means learning that care happens in the small, quiet choices — especially when your body is already carrying enough.
One of the ways I support myself on low-energy days is through gentle, grounding meals that don’t overwhelm the nervous system or digestion.
If your body needs something warm, simple, and supportive tonight, I created something for you.